
Though receiving medical treatment and staying at a hospital isn’t always enjoyable, it’s undeniably necessary. Similarly, being discharged and preparing for your recovery is just as vital to remaining healthy.
There are several important steps everyone should take in order to prepare for being discharged home from the hospital, including:
- Learning about prescribed medication and medical devices
- Arranging ongoing and follow-up care
- Handling necessary documentation
People who will soon be discharged should consider details as well as the more obvious and vital components listed above. Asking questions, arranging transportation, and reviewing financial charges are all tasks that are just as important, however menial they may seem.
Preparing to Be Discharged
Besides the discharge process itself, patients should also consider their ongoing needs. Where they will recover, who will help them, and the extent of the help will all be determined by current and future needs
It may seem like being discharged is easy in comparison to dealing with the hospital stay itself. And in many ways, this is true. However, preparing to be discharged can be challenging in and of itself.
Before you leave, double check to make sure these steps are taken care of:
- Medication – Make sure you understand any new medications, their side effects, and how they may interact with any current meds. Check that the supply and dosage is correct and refill your prescription as directed.
- Equipment Aids – Similar to medication, don’t leave without understanding how any new equipment aids and/or medical devices work and how to properly and safely use them. It’s also wise to learn how to replace them.
- Follow-Up Care – If possible, arrange all of your follow-up appointments, prescription refills, therapy appointments, etc. before being discharged. This way, medical personnel and resources are on call as needed.
- Documentation – Before you leave the hospital, make sure to ask for copies of prescriptions, medical certificates, doctor’s notes, and bills. You should also ask for your recovery and support plan, discussed below.
- Questions – Ask a staff member any and all questions you have about medications, therapy, activities, diet, etc. There are no “silly” or “dumb” questions. Find some way to remember the answers, such as writing them down, recording them, or having another person present who will remember.
- Transportation – Arrange transportation from the hospital to your home through a friend or family member, taxi, hospital transport, etc. Make sure whoever is picking you up knows your discharge date, time, and designated pickup area.
Being discharged involves more than just leaving the hospital. It also encompasses your transition, recovery, and ongoing needs requirements.
All of these details can seem overwhelming, but they can be more easily managed with careful planning and preparation. If you’re reading this article, you’ve already taken the first step to preparing for discharge: research!
Recovery and Support Plan
Before you are discharged, staff should discuss your recovery and support plan, tailored to your needs and requirement support level. The goal of your plan is not only to return you to your previous level of health, but to improve your condition. This plan should cover the following details:
- What treatment and support will be necessary post-discharge
- Who will provide treatment and support and their contact information
- When and how often treatment and support will be provided (and when they need to be)
- How your treatment and care will be monitored
- Financial and payment information, including a list of pending charges
- Hospital personnel and care plan coordinator contact information
In addition to your recovery and support plan and prescription information, you should also be given a letter for your GP. This letter will outline the treatment, support, and future care needs that health officials discussed with you. It’s vital that you provide your GP with this letter as soon as possible.
The Discharge Process
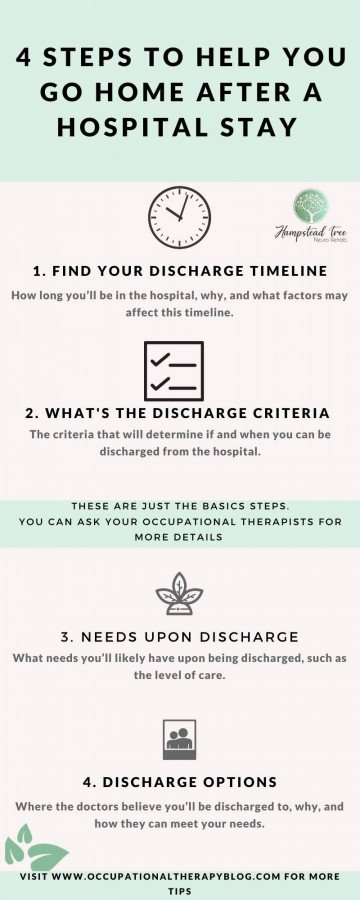
When you arrive at the hospital, the nurse in charge of the ward you’re in will discuss four primary points of care:
- Discharge Timeline – How long you’ll be in the hospital, why, and what factors may affect this timeline.
- Discharge Criteria – The criteria that will determine if and when you can be discharged from the hospital.
- Needs Upon Discharge – What needs you’ll likely have upon being discharged, such as the level of care.
- Discharge Options – Where the doctors believe you’ll be discharged to, why, and how they can meet your needs.
Many patients are discharged from the hospital the same day they arrive, while it takes others weeks or even months to progress through all of these steps.
If you’re dissatisfied with how your discharge is being or was handled, you can contact the staff responsible for your care to try and informally resolve the issue.
If desired, you can escalate the complaint to the NHS Complaints Advocacy service (available through your local council), file a formal complaint via the NHS complains procedure, or leave feedback online about your treatment and discharge.
If you’re confused about your care or discharge at any time, talk to staff as soon as possible and request clarification. Alternatively, you can contact a PALS member, who can offer a variety of services, like advice, general supportive care, and any medical info you may need.
Discharge Timeline
Every patient is different, so there’s no set timeline as to when you’ll be allowed to leave. However, a general rule of thumb is that doctors will discharge you when you no longer need full time hospital care, also called ongoing support.
The staff should discuss your current care needs with you, including how long they expect you to be with them. They should also discuss changes to this timeline that would lengthen or shorten your stay, such as delays in your treatment or unexpected progress.
There are two scenarios in which patients and carers have more control over the discharge timeline:
- Discharging Early – If you so desire, you can discharge yourself against medical advice or earlier than the timeline proposed by your doctor or other staff.
- Discharging Later – If you or someone else feel you’re being discharged too soon, you have the right to appeal the decision and request a review of your current medical standing and needs.
Both of these situations are usually rooted in a disagreement about how ready a patient is to be discharged. Since everyone involved is presumably working in the patient’s best interests, it can be hard to decide who to side with. No matter whether you want to discharge early or later, do your research and consider all the medical benefits and repercussions.
Discharge Criteria
You will not be discharged from the hospital until you no longer need ongoing support. There are a few criteria the doctors will use to assess this, including:
- Whether or not a patient has ongoing medical needs (physical, mental, social, or otherwise)
- The nature and extensiveness of ongoing medical needs and under what conditions those needs can be met
- Whether or not further care will be focused on addressing ongoing medical needs, preventing further medical needs, and/or managing symptoms of medical needs
These criteria may not be applicable to all patients and their specific circumstances. Instead, they serve as a general guideline that many health professionals use when assessing individuals.
These criteria allows staff to evaluate your needs upon discharge and the level of care you’ll require. Patients who needs little to no care are given a minimal discharge. Conversely, patients who require extensive or specialized care are given complex discharges.
Needs Upon Discharge
A patient’s needs upon discharge will largely depend on what medical condition or event prompted their hospital visit and the treatment they received. Though they will vary, some of the more common needs are medication, therapy (physical or other), aid, and/or equipment. Prior to being discharged, an assessment will take place to determine whether or not you’ll need ongoing care after you leave the hospital and how this care will be funded.
For longer term care, your needs after discharge are generally assessed through one of three possible methods:
- NHS Assessments – If you’re eligible, you’ll be assessed through NHS continuing healthcare.
- Local Authority Assessments – Besides NHS, local authorities can also conduct care needs assessments.
- Joint Assessments – Joint assessments are sometimes held to decide whether NHS or local support is more appropriate.
But no matter how you’re assessed, make sure that you are included in the process. Friend and family who you have designated as caregivers can also be a part of the process. Independent advocates are also available for those who need them.
Discharge Options
Your discharge options will depend on your needs and the level of care you’ll need after leaving. Many patients only require minimal assistance with domestic tasks or personal care upon returning home. If necessary, hospitals can arrange immediate care. The doctors may discharge you to several different places, such as:
- Your home
- A residential setting
- A care facility
If you are transferred to either a residential setting or another care facility, it’s likely you’ll need formal care. Once you arrive, you’ll undergo an ongoing support assessment there. Typically, the assessments take place the day you arrive or the day after.
Medications and Appropriate Questions

Medications are often a critical component of the discharge and recovery process. You should be well-informed about the medications you’ve been prescribed, as should any caretakers, friends, family, etc. who will be involved in your recovery.
As such, your doctors and care staff should provide you with detailed explanations of what medications you’ve been prescribed and why. If you have any questions about your medication, you should ask prior to being discharged or as soon as possible.
Common questions about medication include:
- What is the name of the medication (including the “common name”) and how is it spelled?
- What, if any, generic versions are available? How do the prices compare?
- What does the medicine do? What are the possible side effects?
- When should you take the medication? What is the dosage? How should you take it (orally, etc.)? How long should you take it? When will the medicine take effect?
- Under what circumstances should you contact your doctor or stop taking the medication?
- If you’re taking other medications, how will this one interact with it?
- Are there any other medications, foods, activities you need to avoid while on this medication?
- What should you do if you forget to take the medicine or take more/less than the recommended dosage?
And remember: doctors and other staff are there to help you. So, don’t feel embarrassed or otherwise nervous about asking questions. The more you know, the better equipped you are to successfully transition from your discharge and recover.
Considerations for Home Care
The primary consideration if you’re being discharged to your home is who is going to provide for your ongoing needs. Some patients are capable of caring for themselves, but others need the help of family, friends, or professional caretakers.
To decide who can best provide for your needs, consider the following aspects of care:
- Physical Support – Moving around, getting dressed, eating, bathing, etc. are all daily activities that seem insignificant, but which can quickly become stressful
- Emotional Support – Managing anxiety, depression, loneliness, apathy, anger, helplessness, etc. or other mental health issues
- Medical Support – Handling medications, injections, physical therapy, follow-up appointments, equipment aids/ medical devices, etc.
- Housework – Both you and your residence will require care; this includes cleaning, cooking, yardwork, laundry, chores, etc.
- Household Members – If you have children, pets, or other dependents, your care requirements will be compounded by their needs.
An important factor for deciding how much help you’ll need and from whom you want to receive it is the expected timeline for your recovery. Care may be necessary on a short- or long-term basis.
Friends and family may be able to help for a few days of weeks, but professionals are usually more suited to providing help for longer periods of time. Before deciding on a caretaker, you should also consider the toll it will take on them emotionally, physically, socially, and even professionally.
Questions for Residential and Facility Care
If you’re being discharged to a residential environment or to a further care facility rather than your home, there are some questions you can easily ask to learn more about what type of place it is and the quality of care you’ll receive.
- What are the criteria that were/will be used to determine the facility?
- How long are you expected to remain in the facility?
- What are the facility’s ratings online? Is it clean, safe, quiet, and comfortable?
- Does the staff have experience with your needs (medication, therapy, etc.)?
- Is the facility located a convenient or accessible distance from your support system?
- What is the staff turnover rate and how many staff are available at any given time?
It’s possible that you may be moved several times throughout your recovery as medical staff try to find the best fit possible for you. If you have concerns about this process or a specific facility, contact your doctor as soon as possible.
Care Costs
Care costs can quickly jump from affordable to exorbitant depending on your needs and how long you need care for after discharge. Thankfully, there are several scenarios that, if applicable, will make your care more affordable.
- Staff Assessments – Staff will assess your ongoing health and care needs post-discharge and decide how those needs will be funded and how much you’ll have to personally pay.
- New Care Elements – If your recovery and support plan includes new care elements, the government may fund your plan or these specific elements for up to six weeks.
- NHS Continuing Healthcare – If you meet the requirements for the NHS “continuing healthcare”, any further care can be arranged and funded directly by the NHS.
Each of these options and the financial relief they provide will vary depending on individual need and circumstance. For example, NHS covers the cost of care and support for eligible patients discharged to their own home; but if those patients are sent to a care facility, they only cover the associated facility fees.
You should also be prepared for charges that are not covered by social care or other organisations, such as extra services such as cooking, cleaning, managing finances, etc.
Don’t Forget These Steps
Besides everything discussed above, there are a few other steps to remember when preparing to be discharged. These include:
- Gather Necessities – Make sure you have your clothes, toiletries, and house keys. This may also include cash or money depending on your needs.
- Short-Term Care – If you’ll need short-term care, set it up before leaving the hospital to make your transition back home as smooth as possible.
- Stock Up – Whether or not you have a family or friend helping you out, it’s best to stock up on things like food, water, and medical supplies for your recovery period.
- Ask for Notes – If necessary, ask for a doctor’s note or medical information to provide to your insurance companies, employers, and other organizations as required.
If applicable, other steps to take include providing a forwarding address for the post office and arranging for alternate care for your house, kids, pets, work, etc.
Being discharged and preparing to return home can be stressful and time-consuming, so it’s not surprising that sometimes details fall through the cracks. But with these simple reminders, you’ll be ready to leave the hospital with confidence.
Content Disclaimer
The information contained above is provided for information purposes only. The contents of this Blog article are not intended to amount to advice, and you should not rely on any of the contents of this Blog article. Professional advice should be obtained before taking or refraining from taking any action as a result of the contents of this Blog article. OccupationaltherapyBlog disclaims all liability and responsibility arising from any reliance placed on any of the contents of this Blog article.
References
https://www.ageuk.org.uk/information-advice/health-wellbeing/health-services/leaving-hospital/
https://www.ageuk.org.uk/information-advice/health-wellbeing/health-services/nhs-continuing-healthcare/
https://www.nhs.uk/using-the-nhs/nhs-services/hospitals/being-discharged-from-hospital/
https://www.gov.uk/find-your-local-council
https://www.nhs.uk/using-the-nhs/about-the-nhs/how-to-complain-to-the-nhs/
https://www.nhs.uk/Service-Search/Patient-advice-and-liaison-services-(PALS)/LocationSearch/363
https://www.gov.uk/government/publications/leaving-hospital-to-go-home-patient-leaflet
https://www.gov.uk/government/publications/leaving-hospital-to-go-to-another-place-of-care-patient-leaflet
https://www.gov.uk/government/publications/looking-after-friends-or-family-when-they-leave-hospital-leaflet/looking-after-family-or-friends-after-they-leave-hospital
https://www.urmc.rochester.edu/strong-memorial/patients-families/hospital-stay/discharge-preparation.aspx
https://cthosp.org/advocacy/quality-and-patient-safety/patients-guide-to-quality-hospital-care/preparing-for-discharge-from-the-hospital/
https://www.caregiver.org/hospital-discharge-planning-guide-families-and-caregivers

